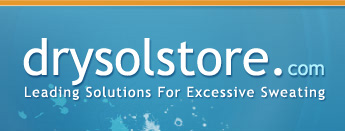
Hyperhidrosis is a medical condition characterized by excessive sweating that goes beyond what the body requires for normal temperature regulation. While most people experience sweating as a natural response to heat or physical exertion, those with hyperhidrosis often face persistent and uncontrollable sweating that can affect various parts of the body, including the underarms, palms, feet, and face. This condition can significantly impact daily life, causing discomfort, social anxiety, and even skin infections if left unmanaged.
Understanding the underlying causes of hyperhidrosis is crucial for effective treatment and symptom management. While many are familiar with common triggers such as heat, stress, or genetics, there are several lesser known factors that can contribute to or exacerbate excessive sweating. Identifying these surprising causes can help individuals and healthcare providers tailor treatment plans more precisely, whether that involves topical antiperspirants, Botox for sweating, or more advanced hyperhidrosis surgery options.
Recognizing the diverse origins of hyperhidrosis also highlights the importance of a thorough hyperhidrosis diagnosis. Some cases stem from primary hyperhidrosis, where excessive sweating occurs without an apparent medical reason, while others are linked to secondary hyperhidrosis, which results from underlying health conditions or medications. By exploring these unexpected causes, individuals can gain a clearer understanding of their symptoms and explore a wider range of treatment options, including specialized antiperspirants or clinical interventions.
For those seeking reliable solutions, resources like hyperhidrosis treatment products can provide effective relief. Whether dealing with excessive palm sweating, underarm sweating causes, or excessive foot sweating, knowing the root causes is the first step toward regaining control and improving quality of life. This comprehensive overview will reveal 10 surprising causes of hyperhidrosis that many people might not realize, empowering readers with knowledge to better manage this challenging condition.

Medical Conditions Linked to Hyperhidrosis
Thyroid Disorders
Thyroid disorders, particularly hyperthyroidism, are a significant yet often overlooked cause of excessive sweating. The thyroid gland plays a crucial role in regulating metabolism, and when it becomes overactive, the bodyís metabolic rate increases dramatically. This heightened metabolism leads to an increase in heat production, which in turn stimulates the bodyís natural cooling mechanism: sweating. As a result, individuals with hyperthyroidism frequently experience excessive sweating that can mimic or exacerbate hyperhidrosis symptoms.
When thyroid hormone levels are elevated, the activity of the hyperhidrosis sweat glands intensifies. These sweat glands respond to the bodyís attempt to dissipate excess heat, but in cases of thyroid imbalance, the sweating can become excessive and persistent, even in cool environments or at rest. This can lead to discomfort and social embarrassment, similar to what is seen in primary hyperhidrosis symptoms, but with an underlying medical cause that requires specific treatment.
Recognizing the overlap between thyroid disorder symptoms and hyperhidrosis is essential for accurate hyperhidrosis diagnosis methods. Symptoms such as unexplained weight loss, rapid heartbeat, tremors, and nervousness often accompany the excessive sweating caused by thyroid dysfunction. Without proper evaluation, patients may be misdiagnosed with primary hyperhidrosis and miss out on targeted treatments that address the root cause. Blood tests measuring thyroid hormone levels are critical in differentiating hyperthyroidism related sweating from other forms of excessive sweating.
Effective management of thyroid related hyperhidrosis involves treating the underlying thyroid disorder. Once thyroid hormone levels are stabilized through medication, radioactive iodine therapy, or surgery, the excessive sweating often diminishes significantly. However, during the period of imbalance, individuals may benefit from adjunctive excessive sweating treatment options such as specialized antiperspirants for hyperhidrosis or Botox for sweating to manage symptoms and improve quality of life.
Diabetes
Diabetes is another medical condition closely linked to episodes of excessive sweating, often complicating the clinical picture of hyperhidrosis. Fluctuating blood sugar levels, particularly hypoglycemia (low blood sugar), can trigger sudden sweating episodes as the body attempts to counteract the drop in glucose. This response is part of the autonomic nervous systemís effort to restore balance, but it can lead to distressing and unpredictable sweating patterns.
In addition to blood sugar fluctuations, diabetic neuropathyóa common complication of diabetesóplays a significant role in excessive sweating. Neuropathy damages the nerves that regulate sweat gland function, leading to abnormal sweating responses. Some patients may experience excessive palm sweating or excessive foot sweating, while others might have reduced sweating in certain areas, creating an uneven and uncomfortable sweating disorder management challenge.
Monitoring symptoms carefully is vital for early diagnosis and effective treatment. Patients with diabetes who report unusual sweating patterns should undergo thorough evaluation to distinguish between primary hyperhidrosis symptoms and secondary hyperhidrosis conditions caused by diabetic complications. This distinction is important because treatment strategies differ significantly. While primary hyperhidrosis may respond well to hyperhidrosis surgery options or Botox for sweating, secondary hyperhidrosis related to diabetes requires comprehensive management of blood sugar levels and neuropathy.
Incorporating hyperhidrosis treatment options tailored to diabetic patients can improve comfort and reduce the risk of skin infections caused by persistent moisture. Antiperspirants for hyperhidrosis, combined with good glycemic control, form the cornerstone of managing excessive sweating in this population. Additionally, ongoing research and hyperhidrosis clinical trials continue to explore innovative therapies that may benefit diabetic patients experiencing excessive sweating.
Parkinsonís Disease
Parkinsonís disease, a progressive neurological disorder, affects the nervous systemís ability to regulate many involuntary functions, including sweat production. Disruption in the autonomic nervous system, which controls sweat gland activity, often leads to abnormal sweating patterns in Parkinsonís patients. Excessive sweating is recognized as a common non motor symptom of Parkinsonís disease and can significantly impact daily comfort and quality of life.
The nervous system disruption caused by Parkinsonís interferes with the bodyís normal thermoregulatory processes. This can result in episodes of excessive sweating that are unpredictable and difficult to control. Patients may experience excessive palm sweating, underarm sweating causes that are unrelated to heat or physical activity, and even excessive foot sweating. These symptoms often coexist with other autonomic dysfunctions such as blood pressure fluctuations and digestive issues.
Understanding sweating as a non motor symptom in Parkinsonís patients is essential for comprehensive care. It requires a multidisciplinary approach that includes neurologists, dermatologists, and specialists in sweating disorder management. Treatment may involve a combination of systemic medications to address Parkinsonís symptoms and localized therapies such as antiperspirants for hyperhidrosis or Botox for sweating to provide relief from excessive sweating.
Because Parkinsonís disease progresses over time, sweating symptoms may worsen or change, necessitating ongoing evaluation and adjustment of treatment plans. Hyperhidrosis diagnosis methods in this context must consider the broader neurological condition to avoid misdiagnosis and ensure that sweating is managed as part of the overall disease process. Patients and caregivers should be aware of the potential for excessive sweating and seek appropriate support to maintain comfort and dignity throughout the course of the illness.

Lifestyle and Environmental Factors
Certain Medications
Medications are a frequently overlooked cause of excessive sweating, and many drugs can induce hyperhidrosis as an unintended side effect. Various classes of medications, including antidepressants, antipyretics, and some cardiovascular drugs, have been reported to stimulate the bodyís sweat glands, leading to increased perspiration. Understanding the relationship between certain medications and hyperhidrosis is essential for effective sweating disorder management and for patients seeking relief from excessive sweating.
The mechanisms by which drugs stimulate sweat glands vary depending on the medication. Some medications affect the central nervous system, triggering the sympathetic nervous system to increase sweat production. Others may directly influence the sweat glands or alter the bodyís thermoregulatory processes. For example, selective serotonin reuptake inhibitors (SSRIs), commonly prescribed for depression and anxiety, can cause excessive sweating by increasing serotonin levels, which in turn activate sweat glands. Similarly, medications used to treat diabetes or hormone replacement therapies may also contribute to hyperhidrosis symptoms.
When excessive sweating is suspected to be medication induced, it is important to consult healthcare providers for alternatives or dosage adjustments. Physicians can evaluate the patientís medication regimen and may recommend switching to drugs with a lower risk of causing hyperhidrosis or adding treatments specifically aimed at controlling sweating. In some cases, combining medication adjustments with hyperhidrosis treatment options such as antiperspirant for hyperhidrosis or Botox for sweating can provide significant symptom relief.
Patients should never discontinue prescribed medications without professional guidance, as abrupt changes can lead to adverse health effects. Instead, open communication with healthcare providers about sweating side effects can lead to personalized treatment plans that balance the management of the primary condition with the need to control excessive sweating. Awareness of medication induced hyperhidrosis is a critical step in comprehensive sweating disorder management.
Stress and Anxiety
Stress and anxiety are powerful emotional triggers that can significantly influence sweating patterns. The connection between these psychological factors and hyperhidrosis is rooted in the activation of the sympathetic nervous system, which controls the bodyís ďfight or flightĒ response. When a person experiences stress or anxiety, this system stimulates the hyperhidrosis sweat glands to produce more sweat, often leading to episodes of excessive palm sweating, underarm sweating, or generalized sweating that can be difficult to control.
Chronic stress exacerbates sweating episodes by maintaining a heightened state of nervous system arousal. Unlike sweating caused by heat or physical exertion, stress induced sweating can occur even in cool environments or during periods of rest. This type of sweating is often unpredictable and can contribute to social discomfort and embarrassment, further intensifying anxiety and creating a challenging cycle. Recognizing the role of hyperhidrosis and anxiety in this feedback loop is essential for effective sweating disorder management.
Addressing stress related hyperhidrosis requires a multifaceted approach. Coping mechanisms such as mindfulness meditation, cognitive behavioral therapy (CBT), and relaxation techniques can help reduce the frequency and severity of stress induced sweating. In addition, medical treatments including antiperspirant for hyperhidrosis and Botox for sweating may be used to manage physical symptoms. Some patients benefit from medications that target anxiety, which can indirectly reduce excessive sweating by calming the nervous system.
Understanding the psychological component of hyperhidrosis is vital for a comprehensive treatment plan. Healthcare providers often incorporate stress management strategies alongside traditional hyperhidrosis treatment options to improve patient outcomes. By addressing both the emotional and physical aspects of excessive sweating, individuals can achieve better control over their symptoms and enhance their overall quality of life.
Caffeine and Diet
Caffeine and certain dietary choices can play a significant role in triggering or worsening hyperhidrosis symptoms. As a stimulant, caffeine activates the central nervous system and increases metabolic rate, which can lead to heightened sweat production. For individuals prone to excessive sweating, consuming caffeinated beverages such as coffee, tea, or energy drinks may provoke or intensify episodes of sweating, particularly excessive palm sweating and underarm sweating.
Beyond caffeine, other foods and beverages can also influence sweat gland activity. Spicy foods, for example, contain compounds like capsaicin that stimulate thermoreceptors in the skin, causing the body to respond with increased sweating as a cooling mechanism. Alcohol is another common dietary factor that can dilate blood vessels and raise body temperature, leading to excessive sweating in susceptible individuals. High sugar foods may also contribute indirectly by affecting blood sugar levels, which can trigger sweating episodes similar to those seen in diabetes related hyperhidrosis.
Managing diet is an important aspect of sweating disorder management for many people with hyperhidrosis. Identifying and reducing intake of dietary triggers such as caffeine and spicy foods can help minimize excessive sweating episodes. Some individuals find that keeping a food diary helps them recognize patterns between their diet and sweating symptoms, allowing for more targeted lifestyle adjustments.
In addition to dietary modifications, combining these changes with hyperhidrosis treatment options such as antiperspirant for hyperhidrosis or Botox for sweating can provide more comprehensive symptom control. Healthcare providers may also recommend hydration strategies and balanced nutrition to support overall health and reduce the impact of dietary triggers on sweat gland activity.
By understanding the influence of caffeine and diet on hyperhidrosis sweat glands, individuals can make informed choices that complement medical treatments and improve their ability to manage excessive sweating effectively.
Other Surprising Triggers
Hormonal Changes
Hormonal fluctuations are a significant and often surprising trigger for hyperhidrosis, influencing sweat gland activity in various stages of life. During puberty, the body undergoes dramatic hormonal shifts that can increase the activity of the hyperhidrosis sweat glands, leading to excessive sweating beyond typical adolescent perspiration. This is largely due to the surge in hormones such as adrenaline and androgens, which stimulate sweat production as part of the bodyís natural response to stress and metabolic changes.
Pregnancy is another period marked by profound hormonal changes that can affect sweating patterns. Elevated levels of progesterone and estrogen, combined with increased blood volume and metabolic rate, often result in heightened sweating. Many pregnant individuals report experiencing excessive underarm sweating causes that are more intense than usual, which can be challenging to manage. These symptoms typically subside after childbirth but can significantly impact comfort and daily activities during pregnancy.
Menopause also plays a critical role in altering sweat gland behavior. The decline in estrogen levels during this phase disrupts the bodyís temperature regulation, often causing hot flashes and night sweats. These episodes of excessive sweating are a hallmark of menopause and can be severe enough to interfere with sleep and quality of life. Understanding the hormonal basis of these symptoms is essential for effective sweating disorder management during menopause.
Managing hyperhidrosis symptoms during hormonal fluctuations requires a tailored approach. Hormone related sweating may respond differently to standard excessive sweating treatment options compared to primary hyperhidrosis symptoms. For example, antiperspirant for hyperhidrosis can provide relief, but some individuals may benefit from additional therapies such as Botox for sweating or lifestyle modifications to reduce triggers. Consulting healthcare providers to address both hormonal health and sweating symptoms ensures a comprehensive treatment plan that adapts to changing physiological conditions.
Genetic Predisposition
Genetics play a crucial role in the development of primary hyperhidrosis, making family history a strong predictor of the condition. Many individuals with hyperhidrosis report having relatives who also experience excessive sweating, indicating a hereditary component that influences sweat gland behavior. This genetic predisposition affects how sweat glands respond to stimuli, often resulting in overactive sweat production without an identifiable external cause.
The influence of genetics on hyperhidrosis sweat glands is complex and involves multiple genes that regulate the autonomic nervous system and sweat gland function. Research suggests that inherited traits may affect the density and sensitivity of sweat glands, leading to the characteristic excessive palm sweating, underarm sweating causes, and other localized symptoms seen in primary hyperhidrosis. Understanding this genetic basis helps differentiate primary hyperhidrosis from secondary hyperhidrosis conditions, which are caused by underlying medical issues.
Recognizing a family history of hyperhidrosis is important for early hyperhidrosis diagnosis methods and treatment planning. Individuals with a genetic predisposition may experience symptoms from a young age and require ongoing sweating disorder management. Treatment options such as hyperhidrosis surgery options, including sympathectomy, or less invasive approaches like Botox for sweating, can be considered based on symptom severity and patient preference.
Genetic counseling and patient education about the hereditary nature of hyperhidrosis can empower individuals to seek timely care and explore the full range of hyperhidrosis treatment options. Advances in hyperhidrosis clinical trials continue to investigate the genetic factors involved, potentially leading to more targeted therapies in the future.
Infections and Fever
Infections and fever are common but often unexpected triggers of excessive sweating. When the body mounts an immune response to fight infection, it frequently raises its core temperature, resulting in fever. Sweating is the bodyís natural mechanism to cool down and regulate temperature during and after febrile episodes. However, in some cases, this sweating can become excessive and persistent, resembling hyperhidrosis symptoms.
Different infections can produce varying sweating patterns. For example, bacterial infections such as tuberculosis are well known for causing night sweats, a form of excessive sweating that occurs during sleep. Viral infections, including influenza and mononucleosis, can also trigger profuse sweating as the body attempts to combat the illness. These sweating episodes are typically temporary but can be intense and disruptive.
In addition to fever related sweating, some infections directly affect the autonomic nervous system or sweat glands, leading to secondary hyperhidrosis conditions. For instance, certain neurological infections or systemic illnesses may alter sweat gland function, causing localized or generalized excessive sweating. Identifying these underlying infections is critical for appropriate hyperhidrosis diagnosis methods and treatment.
Managing sweating related to infections involves treating the primary illness while providing symptomatic relief for excessive sweating. Antiperspirant for hyperhidrosis and other excessive sweating treatment options can help reduce discomfort during recovery. In cases where sweating persists beyond the resolution of infection, further evaluation may be necessary to rule out other causes or complications.
Understanding the role of infections and fever in triggering excessive sweating highlights the importance of a comprehensive approach to sweating disorder management. By addressing both the underlying cause and the symptoms, individuals can achieve better control over their sweating and improve overall well being.
Understanding the Diverse Causes of Hyperhidrosis Enhances Treatment Success
Recognizing the wide range of causes behind hyperhidrosis is essential for effective and targeted treatment. Excessive sweating is not a one size fits all condition; it can stem from a variety of medical, lifestyle, environmental, and genetic factors. By understanding these diverse triggers; ranging from thyroid disorders and diabetes to stress, medication side effects, hormonal changes, and even infections, individuals and healthcare providers can better identify the root cause of symptoms. This comprehensive awareness allows for more precise hyperhidrosis diagnosis methods, which is critical in distinguishing between primary hyperhidrosis symptoms and secondary hyperhidrosis conditions. Such differentiation ensures that treatment plans are tailored to the specific needs of each patient, improving outcomes and quality of life.
Moreover, knowing the underlying causes opens the door to a broader spectrum of hyperhidrosis treatment options. For some, simple lifestyle adjustments or changes in diet may reduce excessive sweating episodes. Others may require medical interventions such as antiperspirant for hyperhidrosis, Botox for sweating, or even hyperhidrosis surgery options. Advances in hyperhidrosis clinical trials continue to expand the possibilities for managing this condition, offering hope for more effective and less invasive treatments in the future. Ultimately, a personalized approach that considers the unique factors contributing to an individualís excessive sweating is the most effective way to achieve lasting relief.
Encouraging individuals to seek professional guidance is a crucial step in managing hyperhidrosis effectively. Consulting healthcare professionals ensures that excessive sweating is properly evaluated and that any underlying medical conditions are identified and treated. Medical experts can recommend appropriate excessive sweating treatment options based on a thorough assessment, including the use of specialized products like Drysol, which are designed to address hyperhidrosis symptoms specifically. These products, combined with professional advice, provide a practical and accessible solution for many sufferers.
Taking the initiative to explore available treatments and working closely with healthcare providers empowers individuals to regain control over their sweating and improve their confidence and comfort. Whether dealing with excessive palm sweating, underarm sweating causes, or other manifestations of hyperhidrosis, professional support and tailored treatment plans are key to successful sweating disorder management. Understanding the complexity of hyperhidrosis and its many triggers ultimately leads to better care and a more manageable, fulfilling life.